In retrospect, it seems hardly possible that the Millennium Development Goals failed to mention tobacco control, but the Framework Convention on Tobacco Control helped ensure a much needed course correction. (1) Today the same might be said of antimicrobial resistance (AMR), a challenge so great that it became only the fourth global health issue ever to be considered by the UN General Assembly.
In the 2016 UN Political Declaration of the High-Level Meeting of the General Assembly on antimicrobial resistance, Member States affirmed that “antimicrobial resistance challenges the sustainability and effectiveness of the public health response to these and other diseases as well as gains in health and development and the attainment of the 2030 Agenda.” (2) Yet the Sustainable Development Goals do not have a single indicator specific to AMR.
AMR places the SDGs at risk
Effective antibiotics remain the cornerstone of modern-day medicine. Organ transplants, surgical prophylaxis, saving newborns from sepsis, warding off infections during cancer chemotherapy—these successes depend on ensuring that these life-saving drugs continue working. An estimated 700,000 die each year from drug-resistant infections. (3) If AMR remains unchecked, the human toll will rise. It is a high-stakes game of Jenga: if antibiotics fail, we will assuredly fall short of attaining SDG 3 (Ensure healthy lives and promote well-being for all at all ages).
Modern medicine – and SDGs 1, 2, 3 and 8, among others – depends on ensuring that life-saving drugs continue working
Worse yet, in so doing, we will also jeopardize the attainment of other SDG goals (see Figure 1). (4) The World Bank has projected that if we do not make sufficient progress on containing AMR, another 24 million people will be pushed into extreme poverty by 2030. (5) , threatening SDG 1 to end poverty in all its forms everywhere. Apart from the impoverishment that comes with illness, another area that is particularly vulnerable to these shocks is livelihoods reliant on livestock production. The interconnectedness of more SDGs with AMR quickly becomes clear. How will these families feed themselves (Goal 2: Zero Hunger), and how will AMR affect their opportunity for employment (Goal 8: Decent Work and Economic Growth)?
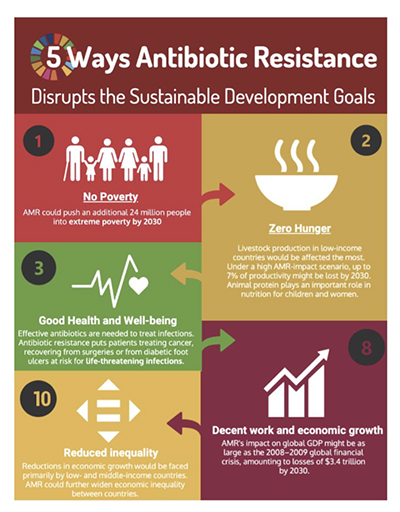
Figure 1: How progress on addressing antimicrobial resistance relates closely to multiple Sustainable Development Goals
AMR-specific tracking within the SDGs is needed
The opportunity to track AMR as part of the SDGs coincides with global attention on the priority of ensuring universal health coverage. (6) Effective antibiotics are an essential building block to delivering universal healthcare. Each year, almost 5.7 million people become ill and die from diseases potentially treatable with antibiotics. (7) The UN Inter-agency and Expert Group on SDG Indicators (IAEG-SDG) has taken up consideration of an indicator proposed by the World Health Organization (WHO) (proposed SDG Indicator 3.d.2) tracking two priority pathogens in bloodstream infections that could serve as sentinels of our progress in addressing AMR. (8) The proposed indicator draws upon a key measure already adopted as part of the WHO’s 13th General Program of Work’s impact framework. (9) Furthermore, the indicator connects with larger efforts afoot in the Monitoring and Evaluation Framework put together by the WHO, Food and Agriculture Organization of the UN (FAO) and the World Organization for Animal Health. (10) As such, it will also help mobilize country-level efforts to bolster their local systems of surveillance.
An OECD analysis studied the potential impact of a hospital-focused intervention that bundled stewardship programs, hand hygiene efforts, and improved environmental hygiene across 33 largely industrialized countries. (11) It found that such an intervention would return a cost savings, after deducting the costs of implementation, of USD PPP 4.1 per capita. Drug resistance rates are even higher in some non-OECD countries. The World Bank similarly concluded in its 2017 report that investing USD9 billion each year in support of both human and veterinary public health systems across 139 countries would yield exceptional returns on investment. (5) While low-income countries would realize significant economic payoffs, the greatest returns would flow to upper middle-income and high-income countries. The improved surveillance efforts spurred by the adoption of an AMR-specific indicator for the SDGs would be invaluable in targeting these investments and monitoring these gains.
Access, but not excess, strikes the right balance
The proposed AMR-specific indicator only captures one side of the coin of antibiotic usage—the risks of potential overuse. However, more people are dying of underuse from lack of access to antibiotics than from drug-resistant infections. (7) So low- and middle-income countries, in particular, deserve to have assurances that we are no less focused on access to these life-saving drugs.
Understandably the IAEG-SDG seeks not to increase unduly the burden of data collection. Fortunately, a couple existing indicators might be adapted to cover this blind spot in the tracking of the SDGs. One of these indicators (SDG indicator 3.8.1) focuses on tracer interventions that address how effectively essential health services are covered. One of these tracer conditions tracks care-seeking behavior for children under five years old with suspected pneumonia. (12) However, the indicator should be enhanced to assess not just whether patients sought care, but received needed antibiotic treatment. The WHO’s 100 Core Health Indicators identified another measure, the Percentage of children who are correctly prescribed an antibiotic for pneumonia, that would accomplish just that. (13)
Even closer to the mark, SDG indicator 3.b.3 follows a basket of tracer medicines for primary health care, four of which are antibiotics. (14) These antibiotics can be categorized under the ACCESS and WATCH groups of WHO’s Essential Medicines List of Access, Watch and Reserve (AWaRe) antibiotics. (15) Both priority pathogens in the proposed AMR-specific indicator—third-generation cephalosporin-resistant Escherichia coli and methicillin-resistant Staphylococcus aureus—require treatment with WATCH group antibiotics. However, where drug resistance rates to WATCH group antibiotics are already high, doctors and patients must turn to RESERVE group antibiotics, which are not currently tracked by this SDG indicator. RESERVE group antibiotics are essential medicines, and their use is increasing. In India, the greatest growth in antibiotic use was seen for RESERVE group antibiotics. (16) Such trends may signal improved availability, but also potentially a need for healthcare systems to steward better these antibiotics. For this reason, we see a need to update the basket of medicines for SDG indicator 3.b.3 to include RESERVE group antibiotics and their use in hospital settings. Alongside local data on rates of drug resistance, this indicator could help tell us which facilities (i.e., hospitals) have needed access to RESERVE group antibiotics for these bloodstream infections. (13) Of course, going beyond access and determining how appropriate these antibiotics are used in such settings would require building out further the methodology of this indicator. Such additional information would offer a snapshot of how healthcare delivery systems strike the right balance between access and stewardship.
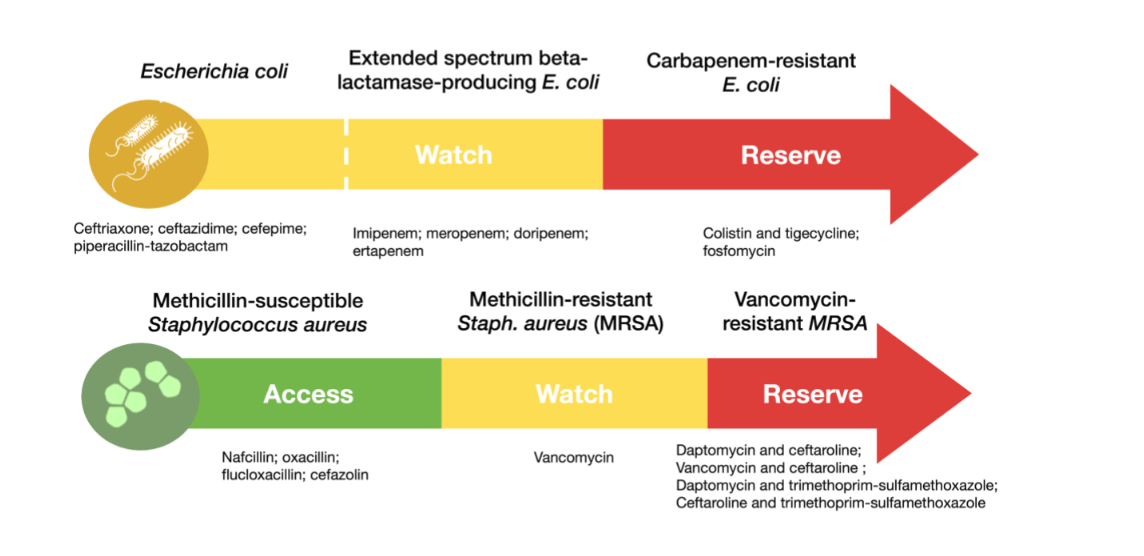
Figure 2: Bloodstream infections tracked by the proposed AMR-specific, SDG indicator require access to RESERVE group antibiotics
Figure description: This diagram depicts the step-up of antibiotics chosen for treatment of bloodstream infections by the priority pathogens in the proposed AMR-specific indicator—Escherichia coli and Staphylococcus aureus. These antibiotics are categorized in the WHO’s ACCESS, WATCH and RESERVE groups. The appropriate antibiotics identified for treatment here are based on suggested regimens in UpToDate. (17,18, 19)
Animal use of antimicrobials also needs monitoring
We would be remiss not to flag the importance of antimicrobial use in the food sector and the need to hold those stakeholders accountable for responsible use of these drugs. In most countries, the majority of antibiotics used, by volume, can be accounted for in food animal production. (20) Furthermore, antibiotic use in food production globally is expected to grow by two-thirds between 2010 and 2030. (21) With future revisions of the SDGs, we hope that indicators capturing the quantity of antibiotics used per biomass, by livestock species, will accompany the indicators of antibiotic use in the healthcare delivery system. Taking a One Health approach will be critical to ensuring that we follow through and go beyond the promise and the recent recommendations of the UN Interagency Coordination Group on Antimicrobial Resistance. (22)
Placing AMR among the indicators tracking our progress on the SDGs is an important steppingstone towards achieving the Global Goals. Even after the IAEG-SDG recommends a revised set of SDG indicators, we will only have ten years remaining to achieve the SDGs before 2030. From the launch of the SDGs, it has taken five years for the global community to consider integrating AMR into the SDGs. Bacteria operate on a much more rapid timescale, and in this game of “Jenga,” the risk of compromising gains made to advance the SDGs is high. Tracking progress on AMR alongside the other SDG indicators is vital for enabling policymakers to understand how AMR affects their own nation’s health, wellbeing and development. With this understanding, each country can undertake cost-saving interventions and services to address AMR and coordinate globally to ensure a future free from the fear of untreatable infections.
References
(1) Esson KM, Leeder SR & WHO Tobacco Free Initiative. The Millennium Development Goals and tobacco control: an opportunity for global partnership. World Health Organization (2004). Available from: https://apps.who.int/iris/handle/10665/43111
(2) Political Declaration of the High-Level Meeting of the General Assembly on Antimicrobial Resistance: resolution. United Nations General Assembly (2016). Available from: https://digitallibrary.un.org/record/845917?ln=en
(3) Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. Review on Antimicrobial Resistance (2016). Available from: https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf
(4) When the Drugs Don’t Work-Antibiotic Resistance as a Global Development Problem. ReAct–Action on Antibiotic Resistance (2019). Available from: https://www.reactgroup.org/wp-content/uploads/2019/02/When-the-Drugs-Don%E2%80%99t-Work-Antibiotic-Resistance-as-a-Global-Development-Problem-Feb-2019.pdf
(5) World Bank. Drug-Resistant Infections: A Threat to Our Economic Future. Washington, DC: World Bank (2017). Available from: http://documents.worldbank.org/curated/en/323311493396993758/final-report
(6) Antimicrobial resistance and universal health coverage – What’s the deal?. ReAct–Action on Antibiotic Resistance (2019). Available from: https://www.reactgroup.org/wp-content/uploads/2019/09/Antimicrobial-resistance-and-universal-health-coverage-Whats-the-deal-ReAct-Sept-2019.pdf
(7) Daulaire N, Bang A, Tomson G, Kalyango JN, Cars O. Universal access to effective antibiotics is essential for tackling antibiotic resistance. The Journal of Law, Medicine & Ethics. 2015 Jun;43(S3):17-21.
(8) Proposals for Consideration in the Open Consultation for the 2020 Comprehensive Review. UN Inter-Agency and Expert Group on SDG Indicators (2019). Available from: https://unstats.un.org/sdgs/files/ope-consultation-comp-rev/Proposals in Open Consultation for 2020 Review.pdf
(9) Thirteenth General Programme of Work, 2019–2023 WHO Impact Framework. World Health Organization (2019). Available from: http://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_5-en.pdf
(10) World Health Organization, Food and Agriculture Organization of the United Nations & World Organisation for Animal Health. Monitoring and evaluation of the global action plan on antimicrobial resistance: framework and recommended indicators. World Health Organization (2019). Available from: https://apps.who.int/iris/handle/10665/325006
(11) OECD. Stemming the Superbug Tide: Just A Few Dollars More, OECD Health Policy Studies (2018). OECD Publishing, Paris, https://doi.org/10.1787/9789264307599-en.
(12) World Health Organization. Metadata for SDG Indicator 3.8.1. UN Statistical Commission (2019). Available from: https://unstats.un.org/sdgs/metadata/files/Metadata-03-08-01.pdf
(13) World Health Organization. 2018 Global reference list of 100 core health indicators (plus health-related SDGs). World Health Organization (2018). Available from: https://apps.who.int/iris/handle/10665/259951.
(14) World Health Organization. Metadata for SDG Indicator 3.B.3. UN Statistical Commission (2019). Available from: https://unstats.un.org/sdgs/metadata/files/Metadata-03-0B-03.pdf
(15) WHO releases the 2019 AWaRe Classification Antibiotics. World Health Organization (2019). Available from: https://www.who.int/medicines/news/2019/WHO_releases2019AWaRe_classification_antibiotics/en/
(16) McGettigan P, Roderick P, Kadam A, Pollock AM. Access, Watch, and Reserve antibiotics in India: challenges for WHO stewardship. The Lancet Global health. 2017 Nov 1;5(11):e1075-6.
(17) Moehring R, Anderson DJ. Gram-negative bacillary bacteremia in adults. Calderwood SB, ed. UpToDate. Waltham, MA: UpToDate Inc. Available from: https://www.uptodate.com/contents/gram-negative-bacillary-bacteremia-in-adults
(18) Quale J, Spelman D. Overview of carbapenemase-producing gram-negative bacilli. Hooper DC, ed. UpToDate. Waltham, MA: UpToDate Inc. Available from: https://www.uptodate.com/contents/overview-of-carbapenemase-producing-gram-negative-bacilli
(19) Fowler VJ, Holland TL. Clinical approach to Staphylococcus aureus bacteremia in adults. Lowy FD, ed. UpToDate. Waltham, MA: UpToDate Inc. Available from: https://www.uptodate.com/contents/clinical-approach-to-staphylococcus-aureus-bacteremia-in-adults
(20) Ritchie H. How do we reduce antibiotic resistance from livestock?. Our World in Data (2017). Available from: https://ourworldindata.org/antibiotic-resistance-from-livestock
(21) Van Boeckel TP, Brower C, Gilbert M, Grenfell BT, Levin SA, Robinson TP, Teillant A, Laxminarayan R. Global trends in antimicrobial use in food animals. Proceedings of the National Academy of Sciences. 2015 May 5;112(18):5649-54.
(22) World Health Organization, Food and Agriculture Organization of the United Nations & World Organisation for Animal Health. No Time to Wait: Securing the future from drug-resistant infections Report to the Secretary-General of the United Nations. World Health Organization (2019). Available from: https://www.who.int/antimicrobial-resistance/interagency-coordination-group/IACG_final_report_EN.pdf
This guest article is written by Anthony D. So, Professor of the Practice at the Johns Hopkins Bloomberg School of Public Health and Director, ReAct Strategic Policy Program, and Prateek Sharma, Research Associate, Johns Hopkins Bloomberg School of Public Health and ReAct Strategic Policy Program
